Heart and cardiovascular conditions are among the most common in the world.
The umbrella term cardiovascular disease (CVD) refers to all the diseases of the cardiovascular system – which consists of the heart and all the blood vessels in the body.
The most common types of heart conditions
Arrhythmia (irregular heartbeat)
An arrhythmia is a type of heart condition where the heart rhythm is not steady. Instead, the heart may feel as though it were skipping a beat, have extra heartbeats every now and then, flutter or race, or beat faster or slower than normal.
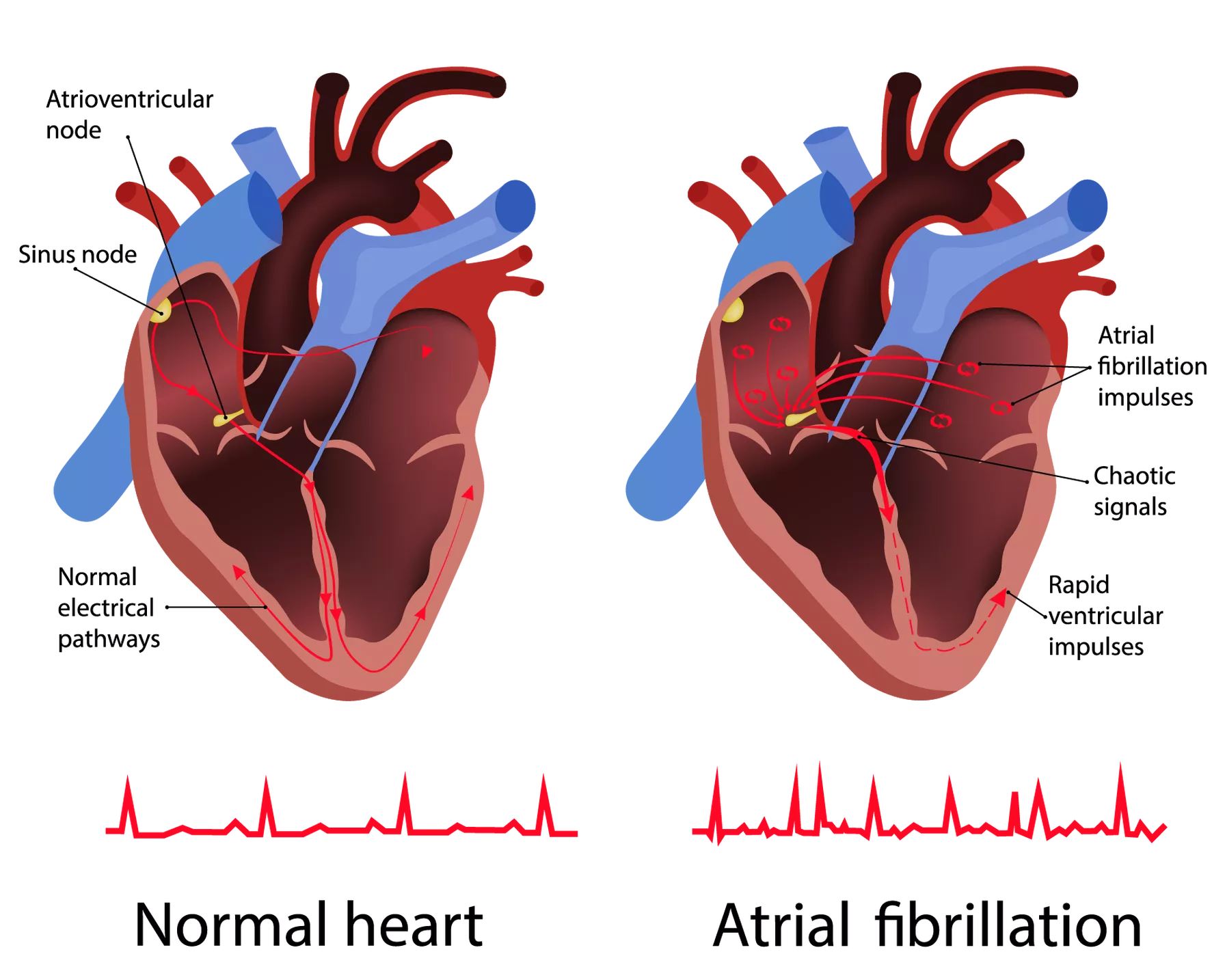
There are many types of arrhythmias, varying in severity and danger. Atrial fibrillation is the most common type. In general, the type of arrhythmia can be categorised by the speed of the heart rate. A normal resting heart rate is regular, with a rate usually between 60 to 100 beats per minute.
Problems with the heart’s rhythm can occur when there is any interruption to the electrical signals that stimulate the heart’s pumping activity. Things that can cause an arrhythmia include other heart conditions such as heart attack or damage from a previous heart attack, heart disease, structural changes in the heart, problems with the thyroid gland, and certain medications and supplements.
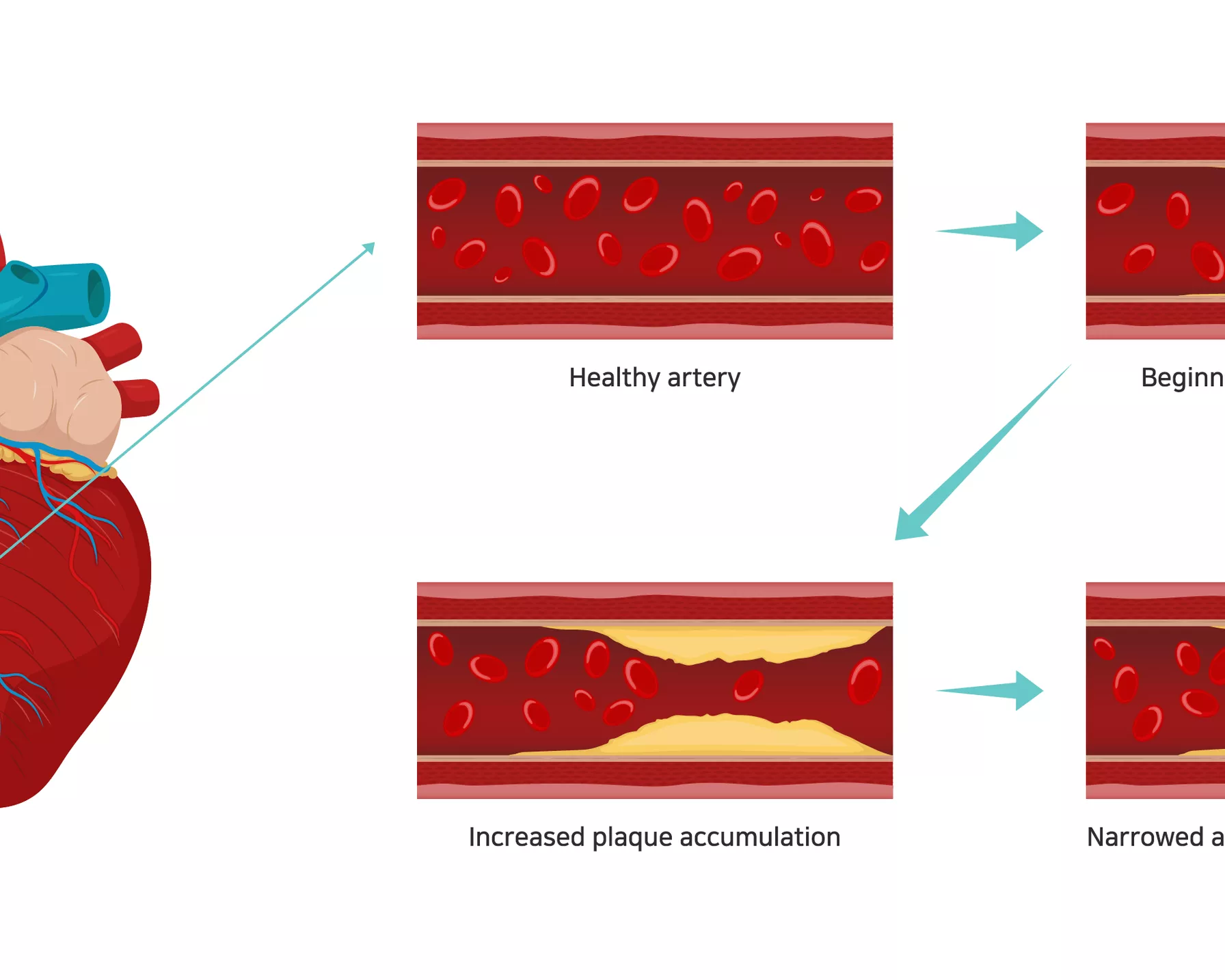
Atherosclerosis
Atherosclerosis is the main underlying cause of CVD. It is a disease in which plaques consisting of fat, cholesterol, calcium and other substances build up in the walls of arteries. Over time, the plaques harden, narrowing the opening of the arteries and restricting blood flow. These atherosclerotic plaques can break, forming a blood clot (thrombosis) that can further limit, or even block the flow of blood throughout the body.
Atherosclerosis can occur in arteries anywhere in the body but is most serious when it occurs in an artery leading to important organs like the heart and brain, as it can lead to a reduced or blocked blood supply.
If atherosclerosis occurs in one of the arteries that supply blood to the heart, it can cause a heart attack. If thrombosis occurs in one of the arteries to the brain, it causes a stroke. If it occurs in arteries in the limbs, it can lead to peripheral artery disease.
The stages of atherosclerosis
Atrial fibrillation
Atrial fibrillation (AF) is the most common type of arrhythmia where the heart beats in a rapid, irregular way, due to a problem in the heart’s chambers. It may not cause any symptoms, or the symptoms may only occur some of the time. It can remain undetected for long periods of time.
While AF is not dangerous in itself, it is important to screen for it and treat it because it increases the risk of other conditions, such as heart failure and stroke. In AF, blood circulates in the heart in an abnormal way, so there is a tendency for thrombosis to occur and blood clots to develop. These clots can break off and travel around the body in the bloodstream. If a clot blocks a brain artery, this can cause a stroke.
Cardiac arrest
A cardiac arrest (also known as sudden cardiac arrest) is when the heart suddenly stops beating. This results in the stoppage of blood flow to the brain and other vital organs, and the sufferer loses consciousness and stops breathing normally.
A cardiac arrest and a heart attack are sometimes used interchangeably, but while both are medical emergencies and can be fatal without immediate treatment, they are not the same.
A heart attack occurs when a blockage stops blood flow to the heart. A cardiac arrest usually occurs when there is a malfunction in the heart’s electrical system that causes the heart to stop beating properly. A cardiac arrest can also be caused by events such as trauma, major blood loss, severe lack of oxygen, electrocution, drowning, allergic reactions and drug overdose. Sometimes the cause of a cardiac arrest cannot be identified.
Congenital heart disease
Congenital heart disease (CHD) is a general term for problems with the heart’s structure that are present from birth. It is also known as congenital heart defect, and it is the most common type of birth defect. It can affect blood flow to the heart and around the body.
There are many different types of CHD, and they can range from simple to complex. CHDs include septal defects (holes in the heart), problems with the blood vessels or heart valves, and single ventricle defects. CHDs can also occur in combination, such as tetralogy of Fallot – a critical CHD where there is a rare combination of four defects of the heart and its blood vessels.
Some CHDs require treatment soon after birth, while some require no treatment. CHDs can have lasting impact, so most people with CHD will need to monitor their heart condition and health in the long term. Regular monitoring as an adult is crucial, as additional treatment or intervention may be needed that was not necessary during childhood. Without proper care, adults with CHD are at increased risk for health concerns such as reduced capacity for exercise, irregular heartbeat and heart failure.
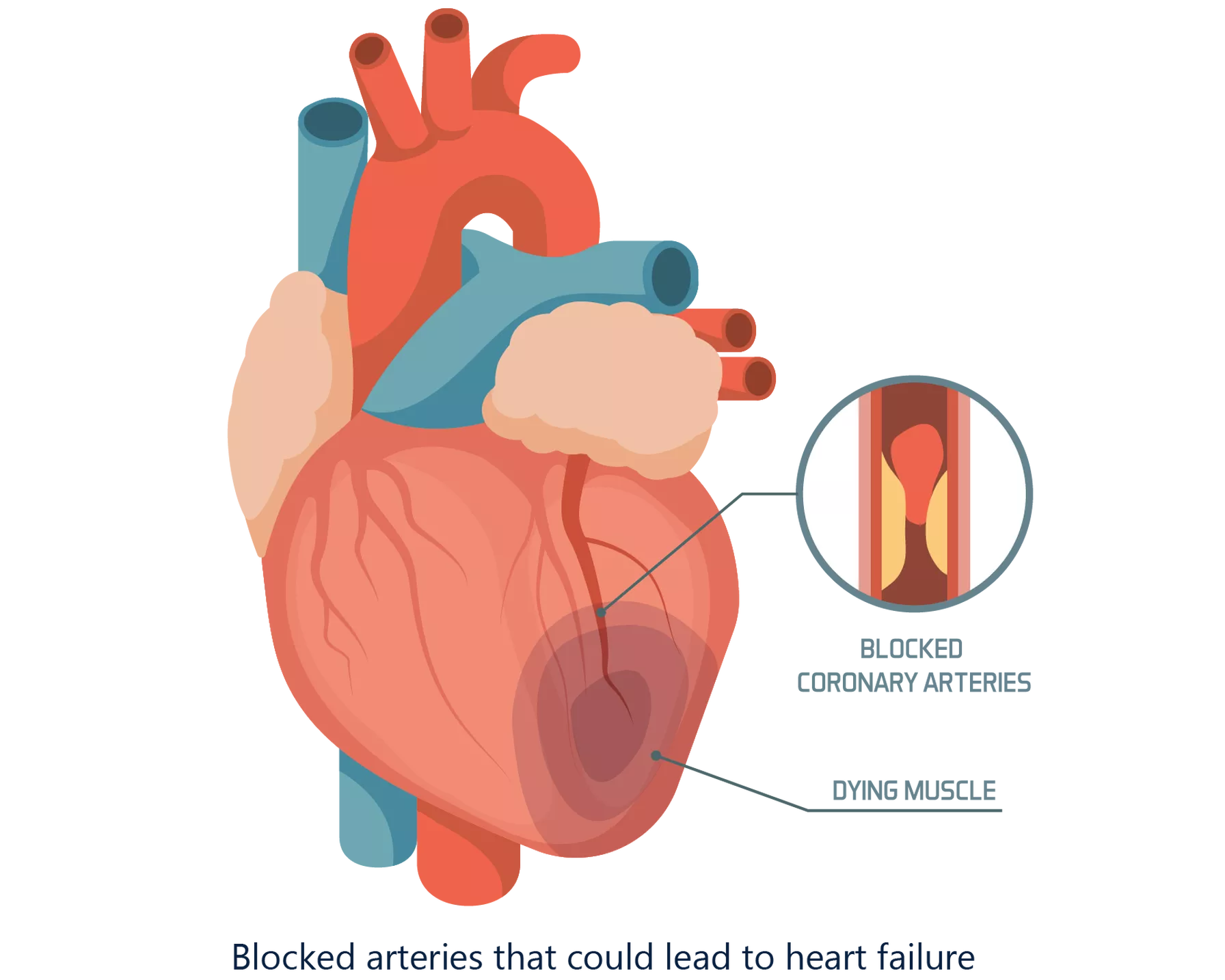
Coronary heart disease
Coronary heart disease is a common condition where the major blood vessels to the heart – the coronary arteries – become blocked and narrowed, restricting the flow of blood to the heart. Coronary heart disease is also known as coronary artery disease.
The main underlying cause of coronary heart disease is atherosclerosis. This is the process by which fat, cholesterol and other substances build up and form plaque in the arteries. If this occurs in the coronary arteries, the plaque can form a blood clot (thrombosis) that restricts the flow of oxygen-rich blood to the heart. Without enough oxygen, the heart cannot function properly, and chest pain (angina) may result. If a blood clot blocks or stops the flow of blood to the heart, it can cause a heart attack.
Coronary heart disease often develops over time. Fatty deposits may develop in the arteries in earlier years and then thicken and build up as the person ages.
The coronary arteries that are affected by coronary heart disease
Diabetes
Diabetes is a condition in which the body cannot maintain healthy blood glucose levels. Insulin, the hormone which regulates these levels, is no longer produced or is not produced in sufficient amounts by the body. Diabetes requires daily management, and it can have a significant impact on quality of life and health, including increased risk of CVD, heart attack, stroke and blindness.
There are three main types of diabetes: gestational diabetes, type 1 diabetes and type 2 diabetes, plus a stage before diabetes called pre-diabetes.
- Gestational diabetes occurs during pregnancy. The body cannot cope with the extra demand for insulin production, resulting in higher than normal blood glucose levels.
- Type 1 diabetes is an auto-immune condition in which the pancreas produces little or no insulin. Those affected need to take insulin every day.
- Type 2 diabetes occurs when the body becomes resistant to the normal effects of insulin and/or gradually becomes unable to produce enough insulin.
- Pre-diabetes occurs when blood sugar levels are higher than the normal range, but not enough to be considered diabetes. People with pre-diabetes are at higher risk of developing type 2 diabetes and CVD later in life.
Heart attack
Heart attack, also known as myocardial infarction, occurs when the heart is deprived of oxygen due to a blocked artery.
When a coronary artery is blocked, the blood flow to the heart is restricted or stopped, reducing the amount of oxygen that the heart receives. Without oxygen, the heart muscle can start to die, and the longer that the blockage remains untreated, the greater the damage to the heart. Without treatment to restore blood flow, the heart can be permanently damaged.
The most common cause of heart attack is coronary heart disease (coronary artery disease), where the blood vessels that supply blood to the heart are blocked by a build-up of fat, cholesterol and other substances that form plaque in the arteries, in a process known as atherosclerosis.
Heart failure
Heart failure, also known as congestive heart failure, is when the heart does not function as well as it should in pumping blood and oxygen around the body. This can damage the organs and cause extra fluid to build up in the body.
Heart failure occurs when the heart muscle becomes too weak to effectively pump blood around the body. It is a long-term condition that usually develops slowly and gets progressively worse (chronic heart failure), although it can occur suddenly. It often develops after other conditions have weakened or damaged the heart, such as coronary heart disease, heart attack and high blood pressure.
A “stiff” type of heart failure called heart failure preserved ejection fraction (HFpEF), where the heart cannot relax properly, is the most common type.
In heart failure, the heart muscle may become damaged and weak, and unable to pump enough blood around the body.
High blood pressure
High blood pressure is very common, with one in three Australian adults living with it.
Also known as hypertension, high blood pressure is when the force of the blood against the artery walls is higher than normal for an extended period of time or the long term. This puts a strain on the arteries, and the heart also has to work harder to keep blood circulating around the body.
High blood pressure is a cause for concern because it can damage the arteries over the long term and is a major risk factor for CVD. It can also cause damage to important organs in the body, such as the brain and kidneys. It’s important to regularly check blood pressure levels so that high levels can be appropriately managed.
| Blood pressure | Systolic (top number) mm Hg | Diastolic (bottom number) mm Hg |
|---|---|---|
| Low | Less than 90 | Less than 60 |
| Optimal | Less than 120 | Less than 80 |
| Normal | 120–129 | 80–84 |
| Normal to high | 130–139 | 85–89 |
| High | Greater than 140 | Greater than 90 |
Preeclampsia
Preeclampsia is a serious condition where high blood pressure occurs during pregnancy and the postpartum period. It affects both the mother and unborn baby, and can lead to maternal and infant death. It generally develops after 20 weeks of pregnancy, although it can develop at any time during the second half of the pregnancy. It is more common in first pregnancies, but it is the most common serious medical complication of pregnancy, affecting one in every 10 women during pregnancy.
If untreated, preeclampsia can lead to serious complications, such as convulsions, kidney or liver failure, and blood clotting problems. In severe cases, preeclampsia can lead to death of the mother or baby. In some cases, the baby needs to be delivered early. Preeclampsia also increases the risk of the mother developing CVD in the future.
Preeclampsia usually resolves after the mother gives birth, and her blood pressure usually returns to normal.
Stroke
Stroke is a leading cause of disability worldwide. It occurs when the blood supply to the brain is suddenly cut off, such as through the blockage or rupture of an artery. If brain cells and tissue do not get enough blood supply, they become damaged and die. Early treatment for stroke is critical – the longer a stroke remains untreated, the greater the chance of stroke-related brain damage.
There are two main types of stroke: ischaemic and haemorrhagic. An ischaemic stroke is when blood flow to the brain is interrupted, such as when a blood clot blocks a brain artery. A haemorrhagic stroke is when a blood vessel or artery in the brain bursts, leaking blood into the brain. Both types of stroke share the same possible signs, symptoms and effects.
How to identify and manage heart and cardiovascular conditions
Different heart and cardiovascular conditions will show different symptoms and be treated or managed in varying ways. It is important to speak to a healthcare professional if you experience symptoms that concern you or have any other concerns about your heart health.
Arrhythmia (irregular heartbeat) symptoms
It is normal for a person to have heart palpitations or a fast or slow heart rate according to their activity and stress levels at the time, but speak to your doctor if the symptoms are ongoing or if you are concerned.
Symptoms of an arrhythmia like atrial fibrillation include:
- fluttering in the chest
- persistent palpitations that feel like pounding
- racing heartbeat
- slow heartbeat
- skipped heartbeats
- chest pain
- shortness of breath.
It you notice signs and symptoms of irregular heartbeat, speak to your doctor to have a check-up.
Treatment will depend on the specific type of irregular heartbeat, its cause, as well as other existing medical conditions. Not all irregular heart rhythms are dangerous or require treatment. Your doctor will determine the treatment plan that will suit your specific situation. This may include medication, medical devices, defibrillation, surgery or lifestyle changes.
Atherosclerosis
Atherosclerosis usually does not cause symptoms until it is at an advanced stage, when the narrowing of arteries becomes so severe that blood flow to the organs and tissues is interrupted or blocked, and CVD has developed. If atherosclerotic plaque that builds up during atherosclerosis breaks and forms a blood clot, it can trigger a heart attack or stroke.
Within the body, a “fatty streak” is the first visible sign of atherosclerosis and indicates the beginning of plaque formation. This fatty streak slowly gets bigger and forms into a larger piece of plaque.
The symptoms experienced during atherosclerosis when it has progressed depend on which arteries are affected. For example, if a coronary artery is affected, chest pain or pressure may be experienced. If a carotid artery to the brain is affected, there may be symptoms of a stroke, such as sudden weakness or numbness in arms or legs, slurred speech or difficulty speaking, temporary vision loss in an eye, or drooping face muscles.
To diagnose atherosclerosis, your doctor may take a complete family and personal medical history and also conduct a physical exam. They may conduct blood tests, angiograms and computerised tomography scans.
Atrial fibrillation
Atrial fibrillation (AF) may not cause any symptoms, or the symptoms may only occur some of the time. AF can remain undetected for long periods of time, which is why it is so important to screen for AF.
Common symptoms of AF include:
- heart palpitations
- racing or ‘fluttering’ heartbeat
- irregular heartbeat, which can be detected by checking the pulse
- pain or discomfort in the chest (angina)
- breathlessness, especially during activity
- dizziness and light-headedness
- tiredness and weakness.
While only your doctor can diagnose AF, you can keep an eye on your heart health by regularly checking your pulse. Keeping a record will help you notice if there is anything different or unusual with your results. Once AF has been diagnosed, medication and other treatments may be prescribed.
The difference between a normal heartbeat and the irregular heartbeat felt in atrial fibrillation
Cardiac arrest
Cardiac arrest usually happens suddenly and without warning. The risk of cardiac arrest increases with age, and men are at higher risk than women. The person suffering cardiac arrest will:
- suddenly collapse
- lose consciousness
- have no pulse
- stop breathing or will be breathing abnormally, such as gasping for air.
Sometimes cardiac arrest can be preceded by other signs and symptoms that are similar to the signs and symptoms of heart attack. These include:
- chest discomfort
- heart palpitations
- shortness of breath
- weakness.
Call 000 straight away if you suspect a cardiac arrest. Without immediate treatment, cardiac arrest can lead to death. In some cases, cardiac arrest can be reversed if treated immediately.
Immediate treatment for a cardiac arrest until more advanced emergency treatment is available includes performing cardiopulmonary resuscitation (CPR). If a defibrillator or automated external defibrillator (AED) are available, they can also be used to improve chances of survival.
Congenital heart disease (CHD)
Congenital heart defects in CHD occur when the heart does not develop normally while the baby is in the womb. There is no known reason for CHD in most cases, although a combination of genetic and environmental factors in thought to play a part, as well as family history.
Some CHDs can be diagnosed during pregnancy, if an ultrasound scan of the baby in the womb indicates signs of CHD. In these cases, specialist ultrasounds may be carried out to confirm the exact diagnosis. These may also be done if there is a family history of CHD or an increased risk. Not all CHDs can be detected this way, particularly mild ones.
Some CHDs are not detected until after the baby is born, such as if the newborn displays signs of CHD like bluish skin. Other CHDs may not be diagnosed until the child is older, even as late as adulthood.
There is no known way to prevent or cure CHD, although there are treatments available that will depend on the type and severity of the defect.
The majority of mild CHDs, such as small holes in the heart that repair themselves over time, do not need any treatment. In some cases, medications may be used to relieve symptoms, improve how the heart works and treat any side effects of the CHD.
In more serious CHD cases, heart surgery may be required, with complex cases potentially requiring many surgeries over many years.
Coronary heart disease
The symptoms of coronary heart disease depend on the severity of the disease. Some people may experience no symptoms, while others may experience mild to severe ones. Symptoms may also become stronger or more frequent as the disease progresses.
Symptoms can come and go, so they may be unrecognised. The common signs and symptoms include chest pain (angina), pain spreading to the arms, shoulder, jaw or neck, shortness of breath and fatigue.
To diagnose coronary heart disease, your doctor may take a complete family and personal medical history, and also conduct a physical exam and medical tests. Tests may include an electrocardiogram (ECG), stress test and imaging scans.
There is no cure for coronary heart disease, but there are treatment options and lifestyle changes that can help to manage the symptoms and reduce the risk of further cardiac events, such as heart attack.
Treatment options include medications to decrease blood clotting, help lower blood pressure, and help reduce cholesterol levels. If the disease has progressed such that blood flow to the heart is blocked, surgery may be required to restore blood flow.
Diabetes
Over 50 per cent of type 2 diabetes cases can be prevented or delayed if lifestyle changes are made early enough, so early diagnosis and management or treatment is vitally important.
Symptoms of type 2 diabetes can include the following, although some people may experience no symptoms.
- Frequent or excess thirst
- Passing more urine
- Feeling tired and lacking energy
- Feeling hungry frequently
- Having cuts that heal slowly
- Itching, skin infections
- Blurred vision
- Unexplained weight changes
- Headaches and feeling dizzy
In the early stages, type 2 diabetes can often be managed by eating a healthy diet and getting regular exercise. Taking medication or insulin as soon as required can also result in fewer long-term complications.
Heart attack
While a heart attack can be sudden, some people experience symptoms and warning signs hours or even days in advance. A heart attack can only be diagnosed by medical tests. It is important to seek medical help immediately if you suspect a heart attack, as early treatment could mean the difference between life and death. Treatment may involve medications or surgery.
Symptoms can differ between men and women, and they may be experienced alone or in combination. The most common symptoms of a heart attack are:
- chest pain, pressure or an aching sensation in the chest or arms that can spread to the neck, jaw or back
- shortness of breath or breathing difficulties
- nausea or vomiting
- heartburn, indigestion or abdominal pain
- light-headedness or sudden dizziness
- feeling faint or anxious
- cold sweats
- fatigue.
Women are more likely to experience symptoms of heart attack unrelated to chest pain, such as:
- discomfort in the neck, jaw, shoulder, upper back or abdomen
- breathlessness and a general feeling of unwellness
- pain, tightness or discomfort in one or both arms
- nausea or vomiting
- heartburn or indigestion
- sweating
- light-headedness or dizziness
- unusual fatigue.
They also tend to have heart attack symptoms more often when resting, or even when asleep, compared to men. Stress can also trigger heart attack symptoms in women.
Heart failure
Heart failure signs and symptoms can vary in severity, and they may come and go. As heart failure worsens over time, more or different signs or symptoms may present themselves.
A key symptom of heart failure is difficulty breathing or shortness of breath. A person suffering this symptom may:
- find physical activity difficult
- wake up in the night due to difficulty breathing
- find it uncomfortable to lie flat, as this can affect the ability to breathe normally.
It is important to seek emergency treatment if any of the following symptoms are experienced. These signs may be due to heart failure, but they can also indicate other serious conditions:
- chest pain
- fainting or severe weakness
- sudden shortness of breath with coughed-up mucus
- a rapid or irregular heartbeat accompanied by chest pain, shortness of breath or fainting.
To diagnose heart failure, your doctor will assess your symptoms, take your medical and family history, and perform a physical examination that may include medical and screening tests such as an echocardiogram, chest x-ray and exercise stress test. These tests can confirm a diagnosis of heart failure and identify the type.
There is no cure for heart failure and it cannot be reversed, making the ongoing research by HRI investigating new therapeutic strategies for stiff heart failure critical.
High blood pressure
High blood pressure is often called a “silent killer” because most people with the condition experience no symptoms. Almost 50 per cent of adults who have high blood pressure are unaware that they have it. This is why it is important to regularly check your blood pressure and know the measurements that are normal for you.
Symptoms of high blood pressure, if they do occur, can include:
- irregular heartbeat
- headaches in the early morning
- nosebleeds
- changes in vision
- buzzing in the ears.
More serious symptoms may present in severe high blood pressure, such as:
- fatigue
- nausea
- vomiting
- chest pain
- muscle tremors
- confusion
- anxiety.
If your blood pressure is higher than normal, or you have other risk factors for cardiovascular disease, it is important to keep an eye on your levels and have them checked more frequently. Your doctor can advise you for your individual circumstances.
Preeclampsia
The defining sign of preeclampsia is high blood pressure and high levels of protein in the urine, although these may not show immediately noticeable signs. The severity of preeclampsia is determined by the level of blood pressure.
In the initial stages of preeclampsia, most women with the condition feel normal and have no obvious symptoms. The first signs of preeclampsia are often detected during routine prenatal visits, which is why regular check-ups during pregnancy that include blood pressure checks are so important.
Early signs and symptoms of preeclampsia include:
- a sudden rise in blood pressure so that levels exceed the initial level at the start of pregnancy
- excess protein in the urine, which can be a sign of kidney damage.
When preeclampsia is caught early, it can be treated and managed. Treatment can include careful monitoring of blood pressure levels and medications to lower blood pressure and manage complications.
The main treatment and only cure for preeclampsia is a planned pre-term delivery of the baby. In some cases, it is safer for the mother and baby to deliver the baby early than to risk prolonging the pregnancy.
Stroke
Stroke can cause permanent or temporary disabilities, and in some cases can be fatal. The longer that a stroke remains untreated, the greater the chance of brain damage and lasting complications. The body parts that are controlled by the damaged areas of the brain will be affected and show signs of stroke.
The most common signs and symptoms of stroke are:
- facial weakness
- arm weakness
- difficulty with speech.
The signs and symptoms of stroke may occur alone or in combination. They can last a few seconds or even up to 24 hours and then disappear.
An easy way to recognise and remember the signs of stroke is to use the FAST test. If someone is showing these symptoms, immediately seek emergency medical treatment.
- Face: Check whether their facial features, such as their mouth, have drooped.
- Arms: Can they lift both arms?
- Speech: Are they having difficulty speaking, eg, slurring their speech? Can they understand you?
- Time: Time is critical if you see any of the above signs. Call emergency services immediately.
Over 90 per cent of people who have a stroke remain without effective treatment, as the only clinically approved drug to treat ischaemic stroke can be used in only a small percentage of patients due to its severe side effects. To address this urgent need, HRI is conducting a world-first trial of a new anti-clotting drug that could potentially be used in all people who suffer a stroke.

Stroke is a medical emergency – the longer that a stroke remains untreated, the greater the chance of stroke-related brain damage.
How is HRI fighting common heart and cardiovascular conditions?
HRI is investigating new ways to prevent, detect and treat common heart conditions and CVD from a variety of different angles.
Our Atherosclerosis and Vascular Remodelling Group focuses on identifying and gaining insights from the genetic and molecular pathways involved in the build-up of plaque in atherosclerosis. These pathways could be used to improve treatments for atherosclerotic plaque.
Our Cardiovascular-protective Signalling and Drug Discovery Group is investigating how to repurpose existing drugs for next-generation therapies for cardiovascular diseases.
Our Clinical Research Group is conducting research into congenital heart disease (CHD), with a focus on young adults living with CHD. Research conducted by the group includes projects designed to improve quality of life and exercise capacity for people living with CHD; improve health outcomes in CHD for young adults, their families and the health system; and establish a unique National Congenital Heart Disease Registry.
Our Coronary Diseases Group is investigating whether the anti-inflammatory drug colchicine can be repurposed to protect against repeat heart attacks. This drug has already proved safe and effective for treating conditions like arthritis and gout.
Our Heart Rhythm and Stroke Prevention Group is investigating how best to screen at scale for atrial fibrillation (AF), which is linked to one third of strokes, to prevent as many strokes as possible.
Our Vascular Complications Group aims to understand the pathogenesis of blood vessel disease in diabetes, and using this knowledge, identify new strategies to improve function and reduce the burden of disease.
Our Vascular Immunology Group focuses its research on better understanding preeclampsia and its impact, as well as the development of new drug treatments for preeclampsia. Preventing preeclampsia could help prevent or reduce the risk of future CVD in women.